fara Australia Patient & Family Information Forum, part 4 of 5
On Feb 29th, 2024 fara gathered the leading FA researchers in the country, brought them to Brisbane and held a forum at UQCCR for them to tell us about their work. I was lucky enough to attend those presentations, but having rewatched them, I realise that I missed much that was presented at the time. Fortunately fara organised for them all to be recorded and you can view them in your own time at https://www.fara.org.au/news/watch-all-presentations-from-our-recent-patient-and-families-information-forum. Alternatively, you can read my summaries of what was presented (three previously, another below and the final one in a few weeks); or check out both video and write-ups and let me know if you think I’ve done a good job!
I’ve previously written a note summarising presentations from Ian Harding, Mirella Dottori, John O’Sullivan, Monique Bueno-Alves, Lucas Tocchini, Liz Soragni and Martin Delatycki. You can find them HERE, HERE and HERE.
The next presentation was from Amy Hulme. Amy works in Mirella’s lab at the University of Wollongong and she described specific work she’s done with cells responsible for proprioception (sensing relative things, like where a limb is in space) or mechanosensation (sensing physical things like that something’s pushing on a sensor in the body, or there’s heat too close by), how efficiently those signals are sent to the brain, and how efficiently signals are sent in response (triggers that’ll cause action to be taken as a result, like “tilt to the left to stay balanced”, or “plan to go to the bathroom” or “move away from the flame”).
These are all issues that affect FAers directly.
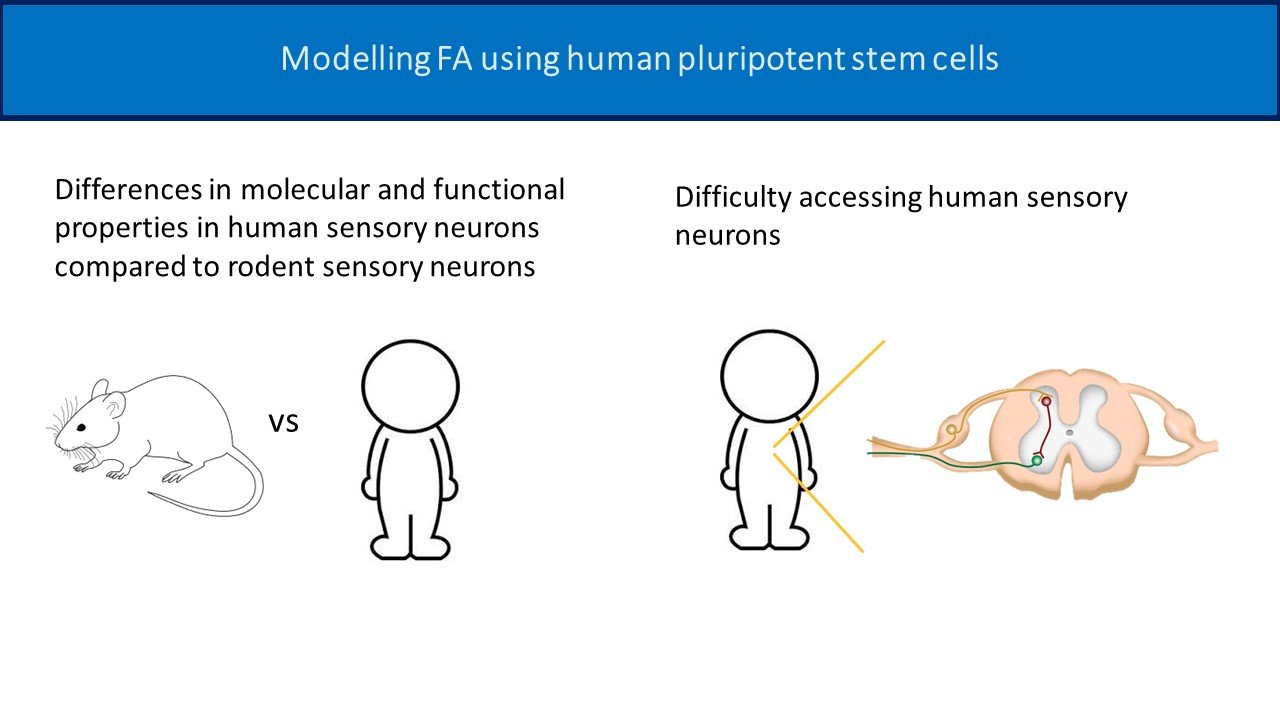
(For a refresher on Mirella’s work, click here.) In Mirella’s lab they work with ips (induced pluripotent stem) cells. Amy’s working on sensory neurons which are a very specialised kind of cell and difficult to isolate. They could be harvested from FA mice but rodents aren’t the same as people. They connect to the DRG (dorsal root ganglia) which is part of the brain – you don’t want to risk damaging someone’s brain harvesting cells to experiment on. Instead, they’ve been able to take skin cells from an FAer, reverse engineer them to become stem cells again, the guide their development so they develop into sensory neurons. Excellent so far, and that’s only where this story starts!
In Amy’s work she was able to prove photographically that she’s got sensory neurons, and then demonstrate how different healthy and FA sensory neurons are. Specifically, she developed a “probe” that can “poke” these neurons and generate a response just like a doorbell. Amy demonstrated both - 1. detect the pressure of the finger on the bell and 2. respond by ringing. I put “probe” and “poke” in inverted commas before because everything we’re talking of here is infinitesimally small!
Importantly, it all worked. Amy can show on a graph that for healthy neurons, when she “pokes” them they respond and that can be repeated again and again, whereas with FA neurons, the same “poking” will elicit a response first time but soon the response will diminish to nothing. (It all fits! Remember that Ian Harding’s work suggested that the FAer’s spinal cord was losing sensory neurons but maintaining motor neurons which is why strength lasts longer for an FAer than control).
Now, as treatments for FA are developed, that they’ll perform as intended can be verified in-vitro before testing on real people. Can Frataxin be added to cells directly? Are other treatments needed? Amy has FA sensory neurons. Treat them, then see how they perform under her “poking” regime!
And now (for you Monty Python lovers out there) for something completely different!
Rucha Sarwade worked until recently at Monash University in Melbourne, with Professor Sureshkumar Balasubramanian and they study plants. Plants? You ask. Yes, plants. Everything we know about genes and genetics started with work done more than 150 years ago by Gregor Mendel with pea plants and Suresh and the team at his SKB Lab know there’s lots more we can learn. They develop models to help that learning, from plants to flies to human cell culture. (Rucha’s moved on but the work continues).
You probably know that FA is characterised by a repeat expansion of the FXN gene (GAA repeated several hundred times in an FAer versus fewer than 50 times in a non-FAer). We know that’s the cause, and we can identify effects (low Frataxin expression, inefficient iron processing, excessive iron-sulphur clusters and free radicals inside the mitochondria, oxidative damage and cell death), but there are difficulties in detailed study of how one leads to the other. There are practical and ethical limits to how we can study FA in living creatures, but there might be valuable parallel learnings we can take from plants.
For example, there’s a plant called Arabidopsis Thaliana that develops a growth defect, and it also has a GAA repeat expansion, in its case, on a gene called IIL1. What’s intriguing though, is that even with the GAA expansion on its IIL1 gene, if it also has a mutation on a gene called FUG1, it can grow healthily.
This suggests a very promising new area for exploration. The work described by Rucha seeks to learn exactly what the effects are of the GAA expansion on the IIL1 gene and if it corresponds exactly with the FXN gene in humans; what exactly is the function of the FUG1 gene and its mutation. Rucha sought to identify the equivalent gene to FUG1 in humans in order that, using CRISPR-CAS9 processes that are already being explored for FA genetic treatments, it can be understood if there’s a different gene therapy treatment path that might be explored for FA.
This is the fourth of a number of these write-ups. Please comment on Facebook or via Contact Us if you find them useful and have comments about any of the research underway. Look out for the next one in another few weeks.