fara Patient Information Forum 2020, note 3 of 3
This is my third and final note documenting what was presented at fara‘s Patient Information Forum in November 2020. It was an information-packed event and I’m delighted I saw it live. Remember, even if you didn’t though, the presentations were all recorded and you can still view them. I’m neither a researcher nor a scientist. This note tells what I, a simple FAer, understood from the presentations. So, as I said before, I still recommend very strongly that you make time to see and hear the full presentations from the researchers themselves.
To view them, click here and when it asks for a passcode, enter: Bbv2Nl=P (that’s a small letter L after the N). Remember, it might appear that only the first 45 minutes is recorded, but when that is finished playing, the recording of the rest appears, as if by magic.
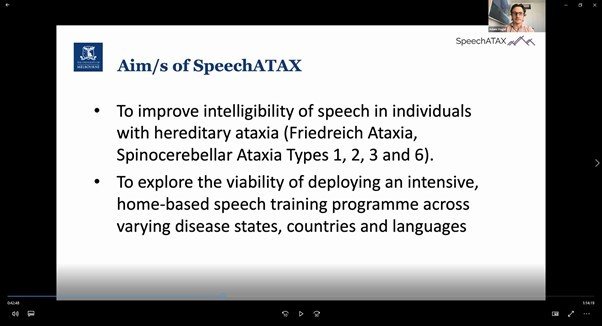
Most of the presentations in this session involved research that’s ongoing and mapped out the theory it’s hoped will be proven as researchers work toward treatments and eventually a cure for FA. Adam Vogel on the other hand, described a project that’s complete (… in fieldwork. Final tabulation of results is just weeks away from being finalised, probably April 2021). He developed, and (it’s likely the final results will show) has proven via a randomised controlled trial, a therapy tool that improves intelligibility of speech in ataxians (FAers and SCAers).
If you didn’t get to participate in that trial, you’ll need to wait while the programme goes through another round of development so it can be used on multiple platforms (it was an Android-only app on Samsung tablet during the trial).
But if you did, and you remember how it all works, you can contact Kristine Evans (kristine.evans1@unimelb.edu.au (Kristine works part time so expect a few days delay before you get a response)) and if you can organise your own Samsung tablet (there might be a delay as we try to sort out the correct specific model), she’ll arrange for you to be able to do it all again.
Next up was Nellie. Nellie Georgiou-Karistianis introduced the TRACK-FA study. This will be a comprehensive study, with a large cohort of (FA and non-FA) participants, over two years at least (baseline, plus follow-ups at 12 months and 24 months), across a number of very different well-established and objectively measureable criteria, using consistent methodology, at six sites (Australia, Brazil and Germany plus 3 x USA). This can then be used as a biomarker set to consistently evaluate clinical trials as the study will generate enough rich data to be able to plot expected results and see how the introduction of a particular treatment changes any of those measures over time. As mentioned in previous notes, having consistent ways to measure criteria is really important in getting FDA (and other regulatory agencies’) approval for new drugs.
Everyone who can (FAers and non-FAers) should participate in this study. There’ll be one initial visit and two follow-ups (12 months and 24 months). Each visit will last up to three hours and include all the tests at one go, including scales, mFARS, brain imaging (MRI), speech etc. Travel and accommodation costs would be covered.
Contact Louise Corben (louise.corben@mcri.edu.au) to confirm if you’re eligible to participate in this study.
Nellie was followed by Ian Harding, who spoke about a study that used a different kind of brain imaging (PET) to measure to what degree neuroinflammation is an issue in FA, how much or when it can be measured and whether it can or should be directly treated.
Inflammation is a normal process employed as part of the immune system that the body uses to flush away dead cells for example. Neuroinflammation is inflammation that happens inside the brain. Normally neuroinflammation is a temporary state but Ian suggests that in many diseases that affect the brain (MS, FA, Parkinson’s, Alzheimer’s etc.), inflammation may be a permanent state and cause harm as a result.
It was confirmed that neuroinflammation is an issue in FA and it’s likely a bigger issue at earlier stages and in those with earlier onset. The theory is that poor production of Frataxin leaves cells vulnerable to oxidative stress and this triggers neuroinflammation and work is ongoing to confirm if that’s the case. If so, then even if the lack of Frataxin can’t be treated, maybe the oxidative stress could be reduced by other means, and some of the damage caused by it avoided as a result.
Ian’s next trial (which will also involve PET scanning in an MRI machine and you might be able to join if you’re signing up for the TRACK-FA study) will study whether oxidative stress measurement can be used to determine whether a drug is having the desired effect more quickly than waiting to see via scales or mFARS after a few months. It could also identify if a drug in a trial is causing more or less response from some FA individuals or others.
Next up was Louisa Selvadurai. Louisa talked through a study that feels like it was a proof-of-concept for the TRACK-FA study. Someone gave Louisa the keys to their MRI machine and she thought to herself “Right, let’s see what this baby can do!” They established a number of measurable criteria and set about measuring them in FAers. They measured the same things in the same number of non-FAers, measured FARS for everyone, then did the same thing two years later so they could establish what changed over time and whether rates of change were significantly different.
The first thing that impressed me with the results was that Louisa started by identifying there were some things they measured that provided no learning at all. To me, that in itself is an important learning.
It served also to clarify that, on other things, there were significant, measurable differences and rates of change over time, between FAers and non-FAers. As always there were inconsistencies between individuals but the study did identify things worth measuring and tracking over time that are most likely to demonstrate significant differences
D’you remember I said a recording had been made of the whole session and you could rewatch it if you’d like? I was wrong. Due to an electronic glitch, Seth Masters’s presentation isn’t there anymore. To understand more about what he’s working on we’ll need to wait until fara‘s next info session.
As a result, I’ll go straight to the presentation from Jarmon Lees. Jarmon’s work is investigating problems and identifying potential solutions in the FA heart. This work is incredibly important because, for all that we’re directly affected by FA’s most obvious symptoms, like balance and coordination issues, dysarthria and poor speech etc., for more than half of all deaths from FA factors, it’s the heart that’s responsible.
Jarmon talked about two areas in which his investigative work is identifying problems specific to FAers and they’ll work to find solutions, and he also shared two visuals that are relevant to his ongoing work, that will stay with me for a long time!
In studying blood vessel cells of FAers, they’ve identified that we’re not good at generating new endothelial cells, the ones that form the walls of blood vessels, closest to blood itself. So they’re exploring ways to encourage production of these cells as more blood vessel production will probably lead to more efficient blood transmission throughout the body and back to the heart and slow down any heart disease.
Separately, they’ve identified what I’ll call “ill discipline” in FAer production of smooth muscle cells. Because we produce too many and they tend to migrate from where they should stay (inside the walls of blood vessels), over time they can cause blood vessels to become blocked. So Jarmon’s group will work on ways to control this migration which should help keep blood flowing smoothly and efficiently.
Of all the cells in our bodies, I personally think cardiomyocytes are probably the coolest. They’re the ones that beat, and they do it when they’re cells in a dish just like they do when they come together to form a heart. I described before how Mirella had tricked cells into being fluorescent. Well Jarmon has cardiomyocytes whose fluorescence turns on as they beat. That lets him measure how rhythmically they beat or, in FAers, the pattern of their irregular beating.
Now he can see what they do wrong, he’ll work on ways to make them better.
And the final image Jarmon left with us is what he referred to as a “cardiac organoid” by which he means a mini-heart, one they’ve created in the lab and can use to verify theories they develop in their research. It’s a real, beating heart, derived from FA iPS cells, only smaller than usual. How small? Well d’you know how an ant can carry its own bodyweight? Yep, an ant could carry the mini-heart!
So that’s it from fara‘s information forum. If ever you meet an FA researcher, your first words should be “Thank you!” They’re doing amazing work. And they kept doing it through 2020 because as we all know, they’re essential workers!